If You Qualify Under A Non
- If you are a U.S. citizen and provide a valid Social Security Number , a match with the Social Security Administration will verify your SSN, date of birth and U.S. citizenship. If SSA verifies this information, no further proof is needed. The SSA match cannot verify birth information for a naturalized citizen. You will need to submit proof of naturalization or a U.S. passport.
- Proof of citizenship or immigration status*
- Proof of age , like a birth certificate
- Four weeks of recent paycheck stubs
- Proof of your income from sources like Social Security, Veteran´s Benefits , retirement benefits, Unemployment Insurance Benefits , Child Support payments
- If you are age 65 or older, or certified blind or disabled, and applying for nursing home care waivered services, or other community based long term care services, you need to provide information on bank accounts, insurance policies and other resources
- Proof of where you live, such as a rent receipt, landlord statement, mortgage statement, or envelope from mail you received recently
- Insurance benefit card or the policy
- Medicare Benefit Card **
Proof of Medicare application can be:
- Your award or denial letter from the Social Security Administration, OR
- Your on-line confirmation letter stating that you have applied for Medicare with the Social Security Administration.
Apply Now:
The following are exempt from all Medicaid co-payments:
Your Protections Under The Newborns And Mothers Health Protection Act
If a group health plan, health insurance company, or health maintenance organization provides maternity benefits, it may not restrict benefits for a hospital stay in connection with childbirth to less than 48 hours following a vaginal delivery or 96 hours following a delivery by cesarean section.
You cannot be required to obtain preauthorization from your plan in order for your 48-hour or 96-hour stay to be covered.
The law allows you and your baby to be released earlier than these time periods only if the attending provider decides, after consulting with you, that you or your baby can be discharged earlier.
In any case, the attending provider cannot receive incentives or disincentives to discharge you or your child earlier than 48 hours .
If your state has a law that provides similar hospital stay protections and your plan offers coverage through an insurance policy or HMO, then you may be protected under state law rather than under the Newborns and Mothers Health Protection Act.
Ways To Apply For Chip:
- Fill out an application through the Health Insurance Marketplace®. If it looks like anyone in your household qualifies for Medicaid or CHIP, well send your information to your state agency. Theyll contact you about enrollment. When you submit your Marketplace application, youll also find out if you qualify for an individual insurance plan with savings based on your income instead. Create an account or log in to an existing account to get started.
FYI: Apply any time
You can apply for and enroll in Medicaid or CHIP any time of year. Theres no limited enrollment period for either Medicaid or CHIP. If you qualify, your coverage can start immediately.
Also Check: How Long Is A Baby Considered A Newborn
May Group Health Plans Insurance Companies Or Hmos Impose Deductibles Or Other Cost
Yes, but only if the deductible, coinsurance, or other cost sharing for the later part of a 48-hour stay is not greater than that imposed for the earlier part of the stay. For example, with respect to a 48-hour stay, a group health plan is permitted to cover only 80 percent of the cost of the hospital stay. However, a plan covering 80 percent of the cost of the first 24 hours could not reduce coverage to 50 percent for the second 24 hours.
Can A Pregnant Woman Receive Medicaid Or Chip Services Prior To An Eligibility Decision
Maybe. States may elect, but are not required, to provide some categories of Medicaid enrollees, including pregnant women, with presumptive eligibility. This allows pregnant women to receive immediate, same-day Medicaid services, typically at the clinic or hospital where they submit an application for Medicaid presumptive eligibility. Currently, 30 states provide presumptive eligibility to pregnant women.
Don’t Miss: How To Get A Newborn Into A Sleep Routine
Do Medicaid And Chip Provide Pregnant Women With Comprehensive Health Coverage
Yes, in most but not all states. Full-scope Medicaid in every state provides comprehensive coverage, including prenatal care, labor and delivery, and any other medically necessary services.
Pregnancy-related Medicaid covers services necessary for the health of a pregnant woman and fetus, or that have become necessary as a result of the woman having been pregnant. Federal guidance from the Department of Health and Human Services clarified that the scope of covered services must be comprehensive because the womans health is intertwined with the fetus health, so it is difficult to determine which services are pregnancy-related. Federal statute requires coverage of prenatal care, delivery, postpartum care, and family planning, as well as services for conditions that may threaten carrying the fetus to full term or the fetus safe delivery. The state ultimately decides what broad set of services are covered. Forty-seven states provide pregnancy-related Medicaid that meets minimum essential coverage and thus is considered comprehensive. Pregnancy-related Medicaid in Arkansas, Idaho, and South Dakota does not meet MEC and is not comprehensive.
CHIP coverage for pregnant woman is also typically comprehensive. However, in states where services are being provided to the pregnant woman by covering the fetus, the services may not be comprehensive with respect to the health needs of the pregnant woman.
When To Contact Your State Medicaid Or Chip Agency
Issues to take to your state Medicaid or CHIP agency include:
- You didnt get an enrollment card and arent sure youre covered
- You cant find a doctor who accepts Medicaid or CHIP, or you cant get an appointment
- You want to know if a service or product is covered
- You have a life change that may affect if youre eligible for Medicaid or CHIP like getting a job that increases your income, your dependent reaching an age where they no longer qualify, or getting married or divorced.
FILLING PRESCRIPTIONS IF YOU DON’T HAVE A CARD: If you need to fill a prescription and havent received your enrollment card yet, check if your pharmacy accepts Medicaid, CHIP, or your health plan. If they do, take your eligibility letter and prescription to the pharmacy. Theyll try to fill it using the information in the letter.
If they dont have enough information, most pharmacies can give you enough medicine for 3 days. Call your Medicaid or CHIP agency or health plan for help getting the rest of your medicine.
If your pharmacy doesnt accept Medicaid, CHIP, or your health plan, call the number in your eligibility letter to find a pharmacy you can use. You can usually find this information on the state Medicaid or CHIP agency website too.
Recommended Reading: How To Help A Constipated Newborn Poop
Can An Uninsured Woman Enroll In A Public Health Insurance Plan Upon Becoming Pregnant
Yes, women who meet the eligibility criteria for Medicaid or Childrens Health Insurance Program can enroll in one of these public programs at any point during pregnancy:
Full-Scope Medicaid
A pregnant woman is eligible for full-scope Medicaid coverage at any point during pregnancy if eligible under state requirements. Eligibility factors include household size, income, residency in the state of application, and immigration status. An uninsured woman who is already pregnant at the time of application is not eligible for enrollment in expansion Medicaid.
Pregnancy-Related Medicaid
If household income exceeds the income limits for full-scope Medicaid coverage, but is at or below the states income cutoff for pregnancy-related Medicaid, a woman is entitled to Medicaid under the coverage category for pregnancy-related services and conditions that might complicate the pregnancy. The income limits for pregnancy-related Medicaid vary, but states cannot drop eligibility for this coverage below a legal floor that ranges from an income of 133% to 185% of FPL , depending on the state. States are permitted to set a higher income cutoff.
Childrens Health Insurance Program
Medicaid In New York State
- COVID-19 News and Updates:
- COVID Information for Medicaid Consumers:
- Medicaid Coverage through Your Local Department of Social Services during the Coronavirus Emergency –
- Medicaid Telehealth Services During the Coronavirus Emergency –
- IRS Form 1095-B Update:
- The 1095-B form for Tax Year 2020 is no longer being mailed automatically.If you need a copy of your 1095-B for Tax Year 2020, you can request it:
- By e-mail – or
Read Also: How Long A Newborn Should Sleep
Important Facts When Having A New Baby
Know your rights. If your plan provides maternity benefits, you should be entitled to a minimum hospital stay of 48 hours following a vaginal delivery and 96 hours following a cesarean delivery.
You cannot be required to get a preauthorization from your plan in order for the minimum hospital stay to be covered.
Your plan must provide you with a notice regarding your rights relating to a hospital stay following childbirth. If your plan is insured, the notice must describe your protections under state law.
Contact your health plan or your spouses health plan as soon as possible to find out how to enroll your new baby in group health plan coverage.
As long as you enroll your newborn within 30 days of birth, coverage should be effective as of your babys birth date, and your baby cannot be subject to a preexisting condition exclusion.
Remember, you should enroll your baby within 30 days of the date of birth.
They Keep Using The Same Card Even After Renewal
How to activate medicaid for newborn in ohio. Fill out an application through the health insurance marketplace®. If it looks like anyone in your household qualifies for medicaid or chip, well send your information to your state agency. Members receive the care and services needed to become and stay healthy.
Well handle all the details for you like contacting your doctor for a prescription and processing the insurance forms. Please fill in the following information. You can buy many health and wellness.
Enroll for my oxaydo ® patient savings program. Helping ohio residents find and apply for benefits. According to medicaid.gov, more than 71 million people are enrolled in medicaid and chip as of september 2017.
Date of birth by using the web portal, mevs, faxback, or avrs. Call your state medicaid or chip agency or your health plan. You have two ways to apply for chip:
You can apply for medicaid coverage in several ways: If you do not see the activation email in your inbox, do one of the following: Ohio department of medicaid | 50 west town street, suite 400, columbus, ohio 43215.
Ohio department of medicaid | 50 west town street, suite 400, columbus, ohio 43215. To buy health and wellness items. There are different ways to apply for ma.
Fill out an application through the health insurance marketplace. You can apply online at benefits.ohio.gov. You may be eligible for medicaid if your monthly income is up to approximately:
Pin on Secret New Board
Pin on
JJaGa on
Also Check: What We Need For Newborn Baby
Important Information For New Or Soon
If you have health coverage and are pregnant, you and your new child may be entitled to a 48-hour hospital stay following childbirth . If your employer or your spouses employer offers a health plan, birth, adoption, and placement for adoption may also trigger a special enrollment opportunity for you, your spouse, and your child, without regard to any open season for enrollment.
The Affordable Care Act adds important protections related to employment based group health plans that will improve health coverage for you and your family. Many of these protections are available now including extending dependent coverage until age 26, prohibiting preexisting condition exclusions for children under 19, and banning lifetime limits on coverage for essential health benefits. Additional protections will be available in 2014. This publication does not reflect the provisions of the Affordable Care Act. For more information, visit the Employee Benefits Security Administrations ACA Web page at dol.gov/ebsa/healthreform.
Frequently Asked Questions For Current Medicaid Beneficiaries
What is a Community Spouse?
A community spouse is someone whose husband/wife is currently institutionalized or living in a nursing home. The community spouse is not currently living in a nursing home and usually resides at the couple´s home.
I am a community spouse. Will I be allowed to keep any income or resources?
If your spouse is institutionalized or living in a nursing home, you will be permitted to keep some income known as a minimum monthly maintenance needs allowance . If you are currently receiving income in excess of the minimum monthly maintenance needs allowance, you may be asked to contribute twenty-five percent of the excess income to the cost of care for the institution
How do I find my local Medicaid office?
The Medicaid office is located in your local department of social services. A listing of offices can be located here:
If you live in the five boroughs of New York City, your offices are run by the Human Resources Administration . A listing of offices can be found here:
How do I order a new benefit card?
If your Medicaid is with your LDSS, to order a new Medicaid Benefit Identification Card, please call or visit your
If your Medicaid is with the and you need to order a new benefit card please call the call center at 1-855-355-5777.
Members residing in the five boroughs of NYC can call the HRA Infoline at 1 557-1399 or the HRA Medicaid Helpline at 1 692-6116.
How often do I have to renew?
Also Check: How To Keep A Newborn Awake During The Day
Medicaid Eligibility And Enrollment: Getting Help With Medicare Costs
July 15, 2021 / 6 min read / Written by Jason B.
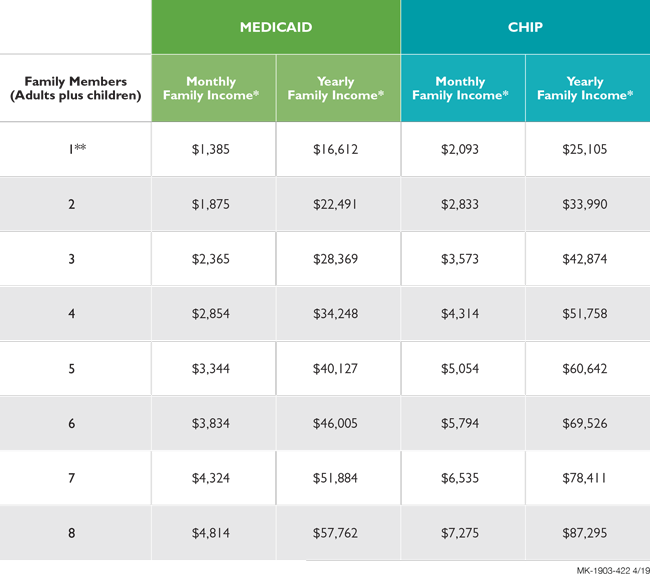
The Medicaid program provides financial assistance with health costs for low-income people, including pregnant women, children, disabled people, and older adults. Medicaid eligibility is limited to United States citizens and lawfully present residents who meet federal and state income and residency requirements.
Medicare beneficiaries with limited incomes may also be eligible for the Medicaid program. These individuals can get help paying for Medicare out-of-pocket expenses, such as deductibles, premiums, copayments, and coinsurance.
Note that health care under Medicaid is not necessarily completely free of charge. There may be costs to you, such as copayments details may vary by state.
State Medicaid eligibility
The federal government partially funds the program and provides minimum requirements for Medicaid income eligibility. However, each state determines Medicaid eligibility for its residents. The state requirements can vary depending on your income and situation.
Most states determine Medicaid eligibility by income and family size with respect to the Federal Poverty Level .The federal minimum eligibility level was $25,100 for a family of four in 2018. In some states, you might qualify for Medicaid if you earn more than the FPL for the number of people in your household.
Medicaid income eligibility may vary by state. You might qualify in your state even if you dont meet the federal minimum requirement.
