What Is The Cdh Survival Rate
The success of CDH treatment often depends upon whether other anomalies are present and a singular survival rate for CDH is hard to determine. Worldwide, the survival rate for CDH has increased over recent decades from 50% to 70 to 80% according to some research. At Children’s Colorado, our team has achieved some of the highest congenital diaphragmatic hernia survival rates in the country, particularly given the severity and complexity of cases we treat. The average survival rate for babies with CDH at Children’s Colorado is 81%.
Improved Outlook For Cdh In Newborns
At Monroe Carell Jr. Childrens Hospital at Vanderbilt, a team led by neonatologist Emily A. Morris, M.D. recently reexamined their congenital diaphragmatic hernia protocol for ways to enhance patient prospects.
Babies born with CDH have a defective diaphragm that allows abdominal organs to herniate into the chest cavity. For these newborns, nuanced decisions on timing and type of treatment typically have amplified outcomes, setting the course for a lifetime of health consequences.
Morris, director of The Fetal Center at Vanderbilt and associate medical director for Childrens Hospitals neonatal intensive care unit , worked with neonatologist Dupree Hatch, M.D., and a multidisciplinary team on a project to enhance and standardize CDH management, both pre- and post-operatively.
We essentially picked up a mirror and looked at our outcomes and use in babies with CDH, and that led us to dig into the literature and see how we could improve, Morris said.
Sixteen babies treated under the new protocol at Childrens Hospital from May 2020 to August 2021 demonstrated improvements in overall survival rates and other measures, Morris said, compared to an earlier cohort. Survival to discharge increased by 19 percent and the number of infants who survived without needing ECMO increased by 39 percent.
What Is The Outcome For A Fetus With Cdh
There is a wide range of severity and outcomes for CDH. In the best cases, some infants do very well with treatment after birth, surgery and care in an intensive care nursery. In the most severe cases, some will not survive no matter how hard we try. And in the middle, some will live normally while others will have a difficult time and may have some handicaps ranging from mild learning problems to breathing and growth problems. How the baby does after birth is determined by how well the lung grows before birth and its function.
Fetuses on the best end of the spectrum have an excellent chance to lead a perfectly normal life. They do not require special prenatal management in terms of the timing or type of delivery, but should be delivered in a perinatal center with a Level III intensive care nursery with neonatal and pediatric surgery support. The place of delivery is very important because transporting these babies after birth can be dangerous for the infant. Babies still need to have the diaphragm hole repaired after birth and will be in the intensive care nursery for several weeks. Even though the lung isnt of normal size at birth, it has the capacity to grow and adapt for many years, so these children can lead normal active lives without restriction.
Don’t Miss: How Much Formula Should My Newborn Eat
Fetal Predictors Of Outcomes
Major determinants of the outcomes in CDH are i) the presence of associated anomalies especially heart disease and ii) extent of lung hypoplasia and position of the liver .
The prognosis of isolated CDH is generally better than CDH complicated by multiple anomalies. Population-based studies report higher survival for isolated CDH compared to CDH with anomalies . Metkus et al. reported higher survival for CDH detected after 25 weeks by ultrasound . This has not been validated and in the true sense, herniation that occurs before 25 weeks tends to have severe lung hypoplasia compared to herniation after 25 weeks .
Liver herniation is associated with worse prognosis. Earlier studies have reported 100% survival without liver herniation as compared to 56% with liver herniation . The survival decreased from 74 to 45% with liver herniation as reported by a meta-analysis . In another study, liver herniation was highly predictive of ECMO and survival .
Metkus et al. used the ratio of the contralateral lung size compared with the head circumference to come up with the lung-to-head ratio to assess the severity of pulmonary hypoplasia and to predict postnatal outcome in fetuses with CDH . Since these measurements differed by gestational age and were not found to be consistent across centers , observed to expected lung-tohead ratio was studied which was independent of gestational age . LHR ratio is often used along with liver herniation to predict outcome
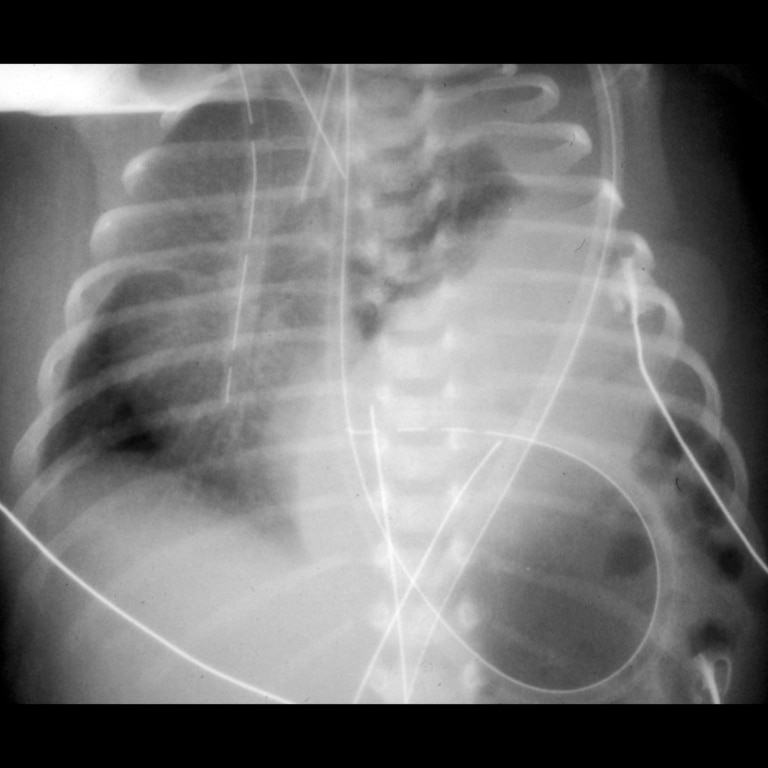
Fig. 6
Fetal Treatment For Cdh
-
Fetoscopic tracheal occlusion : The fetal lungs produce fluid that leaves the body through the babys mouth. If this outflow of fluid is blocked, it has nowhere to go and swells up in the affected lung. When this occurs over a period of four to five weeks, the lung expands and its function appears to improve. This type of blockage can be achieved by temporarily blocking the fetal windpipe with a balloon for a period of time. This is done by performing operative fetoscopy, known as FETO. It is believed that FETO works by increasing the lung maturation and reversing some of the damaging effects of CDH on lung function.
-
Fetal surveillance and delivery planning: There is a high possibility that a baby with CDH will get worse before the anticipated due date. Part of a comprehensive treatment plan will involve close fetal and maternal monitoring to avoid severe fetal deterioration and to determine the circumstances and timing for optimal delivery.
Don’t Miss: How To Potty Train A Newborn
Feto: Prenatal Treatment For Cdh
The Colorado Fetal Care Center specializes in advanced fetal surgery techniques. For the most severe cases of CDH, our MFM specialists may recommend fetoscopic endoluminal balloon tracheal occlusion , a minimally invasive fetal surgery performed to accelerate fetal lung growth. FETO is considered an experimental fetal therapy and not every CDH patient is a candidate for this procedure. At Children’s Colorado, we are one of only eight approved U.S. FETO trial sites in the country.
With FETO, the hope is that the lungs can grow enough that a baby will be able to breathe successfully once they’re born and avoid open fetal or neonatal surgery. Learn more about FETO therapy for severe CDH.
Symptoms Of Congenital Diaphragmatic Hernia
This webpage describes the type of CDH most often found in newborns. Hernias in older children are less severe.
Babies with a CDH may have:
- Serious breathing problems, starting soon after they are born
- Increased work of breathing, for example, using belly muscles to breathe in
- Rapid breathing
Breathing problems happen because:
- Their lungs are smaller than normal.
- Their hearts cannot pump blood easily to the lungs because the walls of the blood vessels are too thick.
- The organs that slip through the hole between the belly and chest are pushing on their lungs.
You May Like: What Is Acid Reflux In Newborns
Treating Congenital Diaphragmatic Hernia
At Seattle Childrens CDH Program, a coordinated team of surgeons, neonatologists, cardiologists, pulmonologists, pediatric intensivists and nutritionists will treat your child. The same team of pediatric surgeons and neonatologists will be involved in your babys care before their birth and throughout their hospital stay. This allows us to get to know your baby very well and give them the very best care.
We felt really loved and cared for they explained everything so well and prepared us for what was to come. He is thriving today, thanks to the incredible care we received at Seattle Childrens over the last nine years. Laurina Barker, mom of Matthew, born with a CDH
Tailored Support For Babies And Families
A more tailored, case-by-case scrutiny extends to all the early decisions made following the babys birth.
Variables may include the size and location of the protrusion, at what stage it developed and its impact on organs pushing into the thoracic chamber. Major physiologic concerns include pulmonary hypoplasia,
systolic and diastolic cardiac dysfunction and pulmonary hypertension.
We need to ask, what is the predominant physiologic bucket for any given baby and how do we safely, and stepwise, try to treat them, she said.
The new protocol also includes new ways of engaging with families in advance of the birth, such as assisting mothers with lactation and designating child life specialists to work with siblings.
This has been extremely well-received by the families, Morris said.
Featured
You May Like: When Can I Put Lotion On My Newborn
Cdh Diagnosis And Evaluation At The Colorado Fetal Care Center
Because CDH might be mistaken for other chest masses, your baby should be evaluated at the Colorado Fetal Care Center, where our expert team can perform a comprehensive prenatal CDH work-up. A full CDH evaluation will include:
- A more detailed fetal ultrasound to understand the significance of the diagnosis
- Fetal echocardiography to evaluate for any accompanying fetal heart conditions
- A fetal MRI to look for any additional abnormalities and measure the size of the lungs, which can help predict the severity of pulmonary hypoplasia
In some cases, we may also recommend an amniocentesis to evaluate the amniotic fluid surrounding you baby. This minimally-invasive fetal diagnostic procedure helps clarify the connection between potential genetic abnormalities and CDH. This is a simple procedure in which we guide a small needle into the amniotic cavity, under ultrasound guidance, and remove amniotic fluid for testing.
Our advanced diagnostic capabilities and CDH expertise allow our experts to not only diagnose your baby’s CDH, but to determine its severity, evaluate for other abnormalities and make recommendations for care before and after birth aimed at ensuring the best outcome possible.
How Does Cdh Affect A Baby After Birth
CDH is a life-threatening defect because it limits the lungs’ growth and can seriously affect a baby’s ability to breathe at birth. These babies will need breathing support as soon as they enter the world. Because of their underdeveloped lungs :
- Newborns won’t be able to take in enough oxygen.
- Not enough blood flows to their lungs.
It’s critical that moms deliver babies diagnosed with CDH before birth in a center that has experience in caring for the complex needs of these vulnerable newborns. Babies with CDH require an all-hands-on-deck approach during the first hours of life.
At the Colorado Fetal Care Center at Children’s Colorado, we have a dedicated CDH team consisting of neonatal and pediatric CDH experts. They specialize in complex delivery planning for babies with CDH, their treatment, management and ongoing care.
Read Also: How To Help Newborn With Gas
Support Groups & Other Resources
- Cherubs The association of CDH research, advocacy, and support. Information, forums, member blogs, and more.
- A Breath of Hope fights lung cancer by funding innovative research and raising awareness through education and patient support
- Researchers, volunteers, educators, outreach workers and advocates working together to give all babies a fighting chance
- Birth Defect Research for Children a parent networking service that connects families who have children with the same birth defects
- Kids Health doctor-approved health information about children from before birth through adolescence
- CDC – Birth Defects Dept. of Health & Human Services, Centers for Disease Control and Prevention
- NIH – Office of Rare Diseases National Inst. of Health – Office of Rare Diseases
- North American Fetal Therapy Network NAFTNet is a voluntary association of medical centers in the United States and Canada with established expertise in fetal surgery and other forms of multidisciplinary care for complex disorders of the fetus.
What Happens After Surgery

After surgery your baby will need continued assistance to breathe effectively. He or she will need frequent lab work to monitor oxygenation, electrolytes and blood counts.
After surgery your baby may need a variety of medications including:
- Antibiotics to fight infection
- Pain medication to control pain after surgery
- Blood pressure medication to stabilize and maintain an adequate blood pressure
- Sedation to keep your baby calm
- Paralytics to keep your baby from moving
Your baby may look puffy or swollen after surgery. He or she will not be able to eat until his or her condition has stabilized. But we will provide nourishment through the IV fluids.
Because infants with this condition cannot eat for a prolonged period of time, we will supply special nourishment through a central line. Total parenteral nutrition is an IV solution that contains protein, fats, sugar, vitamins and minerals. This will supply your baby with all his/her nutritional requirements until he or she is able to take food by mouth.
Read Also: How Many Diapers Does A Newborn Use Per Day
Surgical Repair Of Cdh
Surgical repair of CDH is done through an incision below the rib cage. The time and type of surgery may vary based on the severity and health status of the baby. Medications and inhalation therapies are also given before surgery to enhance lung function. It should be understood that though surgery is a part of long term management it seldom produces acute relief of symptoms.
A Gore-Tex patch or a muscle flap is used to close the diaphragmatic opening, depending on its size. Regular follow-up is done for a few years to observe lung growth in babies.
Congenital Diaphragmatic Hernia : Information For Parents
This publication is licensed under the terms of the Open Government Licence v3.0 except where otherwise stated. To view this licence, visit nationalarchives.gov.uk/doc/open-government-licence/version/3 or write to the Information Policy Team, The National Archives, Kew, London TW9 4DU, or email: .
Where we have identified any third party copyright information you will need to obtain permission from the copyright holders concerned.
This publication is available at https://www.gov.uk/government/publications/cdh-description-in-brief/congenital-diaphragmatic-hernia-cdh-information-for-parents
Also Check: How To Apply For Medicaid For Newborn
What Type Of Surgery Is Performed And When
Surgery to close the hole in the diaphragm is typically performed within two days to two weeks after birth. Open surgery involves a single, longer incision underneath the ribs. Depending on the size of the defect, a synthetic patch may be used to close the hole. In some cases, pediatric surgeons may perform a minimally invasive repair through three or four incisions, each less than 1 centimeter, all near the patients armpit. The appropriate approach will be determined based on each individual patients needs. Overall, the repair operation usually takes about two hours.
The affiliated team will choose the best approach for the individual child. With either approach, the overall goals are the same: reposition the organs that are in the chest back into the abdomen where they belong and rebuild a new diaphragm. Sometimes the diaphragm can be sewn together using sutures only , and sometimes the diaphragm repair requires a special patch to close the diaphragm .
Congenital Diaphragmatic Hernia Overview
In a child with congenital diaphragmatic hernia, the lung on the side of the hole is prevented from growing normally due to the abdominal organs having shifted into the chest area.
The lung on the opposite side is also smaller than expected. Small lungs can also be called pulmonary hypoplasia.
For children with CDH, breathing problems are common at birth. Also, the infants small lungs also have blood vessels that are not developed normally. These vessels are more likely to constrict, making it difficult to get oxygen to the lungs at birth. This causes high blood pressure in the lungs which is called pulmonary hypertension.
There is another problem with the diaphragm that can be similar to CDH called eventration. With an eventration, the diaphragm structure has more fibrous and elastic tissue and less muscle. This makes the diaphragm less effective separating the chest and abdominal contents. As a result, the abdominal organs can move the diaphragm allowing the organs into the chest area. Lung growth is limited on the affected side.
Congenital diaphragmatic hernia occurs in about one in every 2,200 births. About 85% of these defects occur on the left side. CDH can also affect the right side of the diaphragm and, in rare situations, both sides. Overall survival of CDH babies in the United States is approximately 65 70%. At the University of Michigan, however, survival rate is over 80%.
Don’t Miss: How Do You Get Birth Certificate For Newborn
What Does Cdh Mean
- “Congenital” means the defect is present at birth.
- “Diaphragmatic” means the defect affects the diaphragm, a dome-shaped muscular structure that’s just below the lungs and assists in breathing. You can think of a typical diaphragm like a wall that helps keep the contents of the chest separate from the contents of the abdomen .
- “Hernia” refers to the bulging of an organ or tissue through an abnormal opening in the surrounding muscle or connective tissue , one that wouldn’t be there in normal development.
Delivery Room Management And Treatment In The Initial Postnatal Phase
Initial treatment and procedures in the delivery room are based on the updated Guidelines of the International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations .
Monitoring and Goal of Treatment
Measurements of heart rate, pre- and postductal saturations and intra-arterial blood pressure are recommended. The key principles are the avoidance of high airway pressures and the establishment of adequate perfusion and oxygenation . In a study from Dawson et al. in term and preterm healthy neonates, the overall SpO2 values at 10 min after birth were median 94% in preterm infants and median 97% in term infants . Based on expert opinion, the consortium agreed on preductal SpO2 boundaries in the delivery room of 80-95%. In the first 2 h after birth, preductal SpO2 levels as low as 70% are acceptable if they are improving without ventilator changes, if organ perfusion is satisfactory, as indicated by a pH > 7.2, and if ventilation is adequate . Since there is growing evidence that room air is less harmful than 1.0 fractional inspired oxygen in the resuscitation of term infants , it may be better for CDH infants to start with FiO2 lower than 1.0. The aim for preductal saturation is 80-95% after the first hour of life. Thus, to avoid hyperoxia, supplemental oxygen should be diminished by reducing the oxygen fraction when preductal saturation exceeds 95%.
Intubation and Ventilation
Naso- or Orogastric Tube
Vascular Access
Recommended Reading: How To Parent A Newborn
