When The Mother Is Assigned To Sunflower Health Plan:
Delivery and Newborn Claims
- Maternity admissions without delivery complications require notification and information on the delivery outcome within one business day of delivery and must include birth outcomes, including Ballard score or equivalent.
- NICU admissions require notification within one business day of admission. All NICU admissions are subject to concurrent review for continued stay.
For the Mom’s Claim:
Medicaid ID: Use the beneficiary’s Medicaid IDPatient Name: Use the mom’s first and last nameDate of Birth: Use the mom’s date of birthDiagnosis Code: Use the appropriate ICD10 diagnosis code, for example, Z37 –Outcome of Delivery*Room & Board Revenue Code: Use the appropriate Med/Surg/Gyn/OB revenue code
*Note: Z37 ICD10 codes are not for use on the newborn claim
Will A Marketplace Health Plan Also Cover A Newborn
Yes. The ACAs EHB requirement mandates coverage of maternity and newborn care. Newborn care covers childbirth and immediate care for the baby after birth. The specifics of this coverage will vary by state and by each individual plan, but all women in Marketplace coverage must also enroll their baby in coverage soon after birth.
If the newborn is eligible for Marketplace coverage, then the parents can choose to add the baby to the familys existing Marketplace plan or choose a new Marketplace plan for the baby. If they opt for the latter, they can enroll the baby into a new Marketplace plan at any metal tier. However, when enrolling a newborn into Marketplace coverage, other members of the household are generally not permitted to change their existing Marketplace coverage.
Monitoring Substitution Of Coverage In Chip
States are required to include in their state plan a description of procedures used to ensure that CHIP coverage does not substitute for coverage under group health plans. States use various procedures to prevent substitution of coverage, such as monitoring survey data or private insurance databases, or applying a waiting period for individuals who are no longer enrolled in private coverage. This requirement can be found at section 2102 of the Social Security Act. Additional information on states specific CHIP waiting period policies.
Recommended Reading: Does Gripe Water Help With Constipation In Newborns
Does Private Insurance Also Cover A Newborn
It depends. Small group employer-sponsored plans must include the EHBs, including maternity and newborn care, but large group and self-insured employer-sponsored plans are exempt from this requirement. While the requirement for newborn care covers childbirth and immediate care following birth, women must enroll their babies in coverage soon after birth.
How To Apply For Social Security Benefits
If you think your baby may qualify for SSI benefits, you should apply as soon as you are able. Although it can take up to three to five months for the Social Security Administration to decide eligibility for most children with disabilities, it will grant SSI immediately to families of babies who weigh less than 2 lbs 10 oz at birth. However, other preemies with low birth weight or babies with growth failure after birth won’t receive SSI payments until the application and review processes are complete.
Your infants birth weight must be documented by an original or certified copy of the birth certificate or in a medical record signed by a physician. If your child fails to grow as expected and has developmental delays, it’s important to collect and submit regular doctor’s records with your application.
To apply for SSI benefits, you can visit your local social security office or call the Social Security Administration at 1-800-772-1213. Also, don’t hesitate to check if the hospital where you delivered your baby can help many neonatal intensive care units have representatives who are pros at guiding parents through the SSI application process.
If you have applied for and received immediate SSI relief for your baby with low birth weight and it’s determined that your baby doesn’t meet all the requirements for disability benefits, after all, you won’t have to pay back any payments you received to that point.
Don’t Miss: What Do Newborns Need The Most
Medicaid And Your New Baby
If you have a baby while you are on Medicaid or ARKids First, your baby will most likely be able to get Medicaid too.
You need to fill out paperwork on your new baby as soon as you can.
- Go to the DHS office in your county, or
- Fill out an application on the Internet.
Youll need a birth certificate or some kind of proof of your babys age.
Make sure your baby sees the doctor for well-child check-ups and shots. If your baby has Medicaid or ARKids First, these services are paid for. Talk to your doctor about how often your baby needs well-child check-ups.
Other Financial Assistance Programs
If you have a preemie or baby with weight and growth problems and lack private insurance, there are other ways to get some financial relief to help curb costs for their care. These programs include:
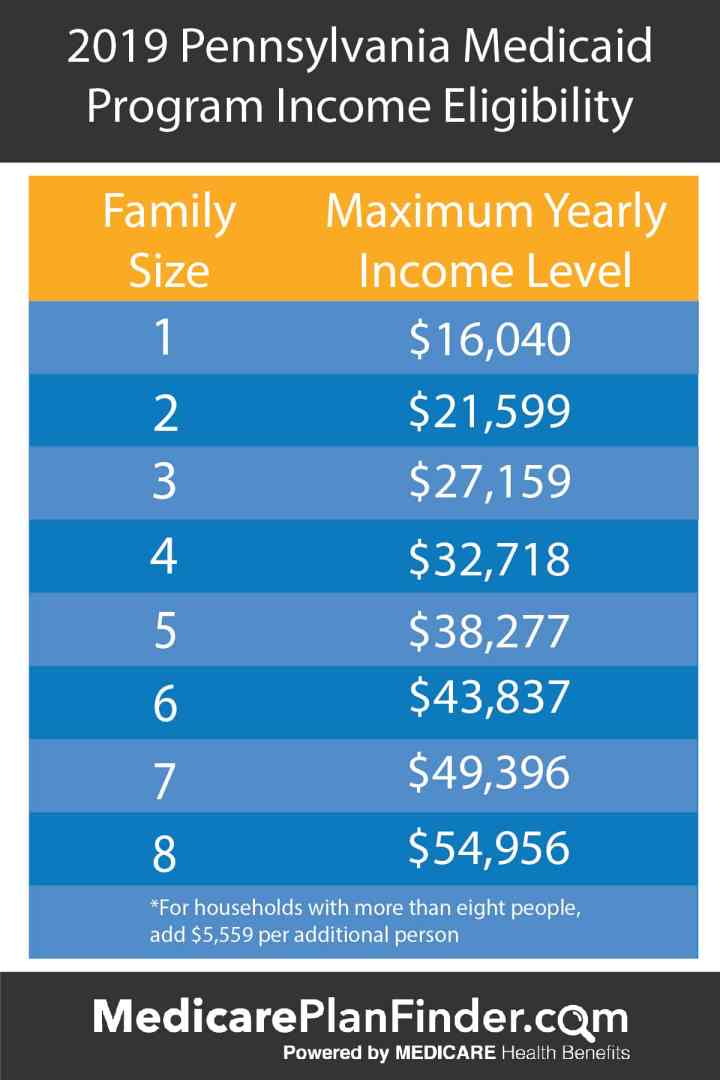
- Medicaid: Depending on the state, a family who qualifies for SSI on behalf of a child may also qualify for Medicaid, a healthcare program for low-income people. Even if your child doesn’t qualify for SSI, they might be eligible for Medicaid and other state and local programs. Check with your state Medicaid office and your state or county social services.
- CHIP: The Children’s Health Insurance Program covers medical and dental costs for millions of kids whose families aren’t insured otherwise. You can apply for coverage and find participating doctors on the federal Insure Kids Now website.
- WIC: Managed by the United States Department of Agriculture , the Supplemental Nutrition Program for Women, Infants, and Children is designed to promote the health of expecting parents along with children up to age 5. To meet WIC eligibility for these monthly food vouchers, families must have an income at or below the poverty line and have demonstrated nutritional needs or deficiencies.
Also Check: How Long Do You Sponge Bathe A Newborn
If You Dont Have Health Coverage
- Health coverage makes it easier to get the medical check-ups and screening tests to help keep both you and your baby healthy during pregnancy.
- If you qualify for a Special Enrollment Period due to a life event like moving or losing other coverage, you may be able to enroll in a Marketplace health plan right now. Being pregnant doesnt make you eligible, but the birth of a child does.
- Create an account now to apply for Marketplace coverage through the Open Enrollment Period or a Special Enrollment Period. If you select the option to get help paying for coverage on your application, youll be asked if youre pregnant. Reporting your pregnancy may help you and your family members get the most affordable coverage.
- If you dont qualify for a Special Enrollment Period right now, youll be eligible to apply within 60 days of your childs birth. You can also enroll in 2021 coverage during the next Open Enrollment Period this fall.
- If eligible for Medicaid or CHIP, your coverage can begin at any time.
Can Uninsured Women Enroll In Marketplace Coverage Upon Becoming Pregnant
Only if it is within the established open enrollment period or a woman qualifies for a special enrollment period , does not have a plan that meets MEC through Medicaid or an employer, and meets income and immigration criteria. Note that except in the states of New York and Vermont, pregnancy does not trigger an SEP.
Under the ACA, people who do not qualify for Medicaid coverage that meets MEC, and have incomes between 100% and 400% FPL, qualify for advance premium tax credits and cost-sharing reductions , which they can use to reduce the cost of health insurance purchased through a Marketplace. Those with pregnancy-related Medicaid in the three states that do not constitute MEC are eligible for Marketplace subsidies. Certain lawfully-present immigrants with incomes under 100% FPL subject to Medicaids five-year ban in their state are also eligible for APTCs. Undocumented immigrants are not eligible for APTCs, CSRs, or Marketplace insurance.
Also Check: What Are The Signs Of Colic In Newborns
Can Uninsured Immigrant Women Receive Medicaid Or Chip Services
Maybe. Immigrants with qualified non-citizen status are eligible to enroll in Medicaid if they otherwise meet state Medicaid eligibility requirements, but are subject to a five-year waiting period from the time they receive their qualifying immigration status before becoming eligible. Some categories of qualified non-citizens are exempt from the five-year ban because they are considered lawfully residing immigrants. For lawfully residing immigrants, the five-year waiting period was waived in 2010, giving states the option to provide lawfully residing immigrant women with pregnancy-related Medicaid regardless of the length of time they have been in the U.S. Twenty-three states provide pregnancy-related Medicaid to lawfully residing immigrants without waiting periods. For undocumented and DACA-eligible immigrants, states may provide undocumented immigrant women with federally funded prenatal services through CHIP. Some states may also provide prenatal care entirely using state funds.
How Can I Determine If I Qualify For Medicaid
Qualifying for Medicaid is not as black and white as qualifying for most other government programs. Most government programs have some basic requirements along with very clear income guidelines to help individuals know if they qualify.But Medicaid has many ways that someone can qualifyand even though income makes up part of the eligibility requirements, it is not solely based on that. Even people with the lowest incomes may not qualify for Medicaid if they do not fall into one of the Medicaid groups.
And people who make a middle-range income may qualify if they fit one of the qualifying groups and can fall back on options such as share of cost
If you are pregnant and uninsured, Contact your local Medicaid office to find out if Medicaid is the right option for you.
Compiled using information from the following sources:
1. US Government Information
Don’t Miss: What Rights Does A Father Have To A Newborn Baby
What Services Are Covered
Medicaid covers breast pumps and breast feeding support during your pregnancy and after your baby is born.
You will get health care services through health plans. The health plans all have special programs for high-risk pregnancies. To learn more, go to Health Plan Information. Or call your health plan.
When Billing For A Newborn Who Has Their Own Medicaid Id Number:
For the Baby’s Claim:
Medicaid ID: Use the newborn’s Medicaid IDPatient Name: Use the newborn’s first and last name as shown in KMAP or on the ID cardDate of Birth: Use the newborns date or birth|Diagnosis Code: Use the appropriate ICD10 diagnosis code, for example, Z38 –Liveborn Infants according to place of birth and type of delivery**Room & Board Revenue Code: must be a nursery room and board revenue code 170-179
**Note: Z38 ICD10 codes are not for use on the mother’s claim
Also Check: Why Is Newborn So Fussy
How To Apply For Medicaid
Virginia Medicaid accepts applications for health coverage year-round. You can choose from three different ways to apply:
Visit CoverVa.org for more information:
Health First Colorado Regional Organizations Frequently Asked Questions
What is changing about Health First Colorado?
Health First Colorado is working to improve the delivery of services. Starting July 1, 2018, Health First Colorado began contracting with one organization in each region of the state to manage both your physical and behavioral health care.
What is a Health First Colorado regional organization?
Your regional organization manages both your physical and behavioral health care. They support a network of providers to make sure you can access health care for your body, vision, mental health, and substance use in a coordinated way. Every Health First Colorado member belongs to a regional organization. Your regional organization is on your enrollment letter.
What is a regional organization and why are they involved in my health care?
Health First Colorado contracts with regional organizations to manage both your physical and behavioral health care. They support a network of providers to make sure you can access health care for your body, vision, mental health, and substance use in a coordinated way. Every Health First Colorado member belongs to a regional organization. Your regional organization is on your enrollment letter.
I’ve been a Health First Colorado member for years and I have never been contacted by a regional organization. I’ve never even heard of them. Why is that?
What will the regional organization do exactly? How will they be involved?
What is a managed care plan? How is it different from Health First Colorado?
Recommended Reading: When Do You Wash A Newborn
Is It Illegal For A Child Not To Have Health Insurance
Unless you qualify for an exemption, you will be subject to a tax penalty for any month you are not covered under a qualified health plan. The Tax Penalty for 2018 is 2.5% of your total household Adjusted Gross Income, or $695 per adult and $347.50 per child.
Frequently Asked Questions For Current Medicaid Beneficiaries
What is a Community Spouse?
A community spouse is someone whose husband/wife is currently institutionalized or living in a nursing home. The community spouse is not currently living in a nursing home and usually resides at the couple´s home.
I am a community spouse. Will I be allowed to keep any income or resources?
If your spouse is institutionalized or living in a nursing home, you will be permitted to keep some income known as a minimum monthly maintenance needs allowance . If you are currently receiving income in excess of the minimum monthly maintenance needs allowance, you may be asked to contribute twenty-five percent of the excess income to the cost of care for the institution
How do I find my local Medicaid office?
The Medicaid office is located in your local department of social services. A listing of offices can be located here:
If you live in the five boroughs of New York City, your offices are run by the Human Resources Administration . A listing of offices can be found here:
How do I order a new benefit card?
If your Medicaid is with your LDSS, to order a new Medicaid Benefit Identification Card, please call or visit your
If your Medicaid is with the and you need to order a new benefit card please call the call center at 1-855-355-5777.
Members residing in the five boroughs of NYC can call the HRA Infoline at 1 557-1399 or the HRA Medicaid Helpline at 1 692-6116.
How often do I have to renew?
Also Check: Do Newborn Babies Cry A Lot
Who Is Eligible For Medicaid
The general guidelines for eligibility for Medicaid are set by the Federal government however, each state sets up their own specific requirements for eligibility and these can differ from state to state.
All States are required to include certain individuals or groups of people in their Medicaid plan.
The state eligibility groups are:
- Categorically needy
- Medically needy
- Special groups
In the categorically needy group, this will cover pregnant women whose income level is at or below 133% of the Federal Poverty level.
In the medically needy group, this will cover a pregnant woman who makes too much money to qualify in the categorically needy group. This means that women, who may have been denied Medicaid before, may be able to qualify now.
