Pregnant Women And Infants
Healthy Connections provides coverage to pregnant women with low income. This coverage for the mother continues for 60 days after the baby’s birth. The infant is covered up to age one.
A woman who may qualify for this program must:
- Be pregnant
- Be a South Carolina resident
- Be a U.S. citizen or Lawful Permanent Resident Alien
- Have a Social Security number or verify an application for one
Individuals who are eligible will receive all Medicaid covered services.
Apply online or complete the following form and submit it electronically to , by mail to SCDHHS-Central Mail, P.O. Box 100101, Columbia, SC 29202-3101 or to your .
The Omnibus Budget Reconciliation Act of 1986 gave states the option to provide Medicaid coverage to pregnant women with low income.
Will A Marketplace Health Plan Also Cover A Newborn
Yes. The ACAs EHB requirement mandates coverage of maternity and newborn care. Newborn care covers childbirth and immediate care for the baby after birth. The specifics of this coverage will vary by state and by each individual plan, but all women in Marketplace coverage must also enroll their baby in coverage soon after birth.
If the newborn is eligible for Marketplace coverage, then the parents can choose to add the baby to the familys existing Marketplace plan or choose a new Marketplace plan for the baby. If they opt for the latter, they can enroll the baby into a new Marketplace plan at any metal tier. However, when enrolling a newborn into Marketplace coverage, other members of the household are generally not permitted to change their existing Marketplace coverage.
Can An Uninsured Woman Enroll In Marketplace Coverage Upon Giving Birth
Maybe. If the baby is eligible for Marketplace coverage, then the baby qualifies for an SEP as a new dependent. In such instances, the regulations will also permit an SEP for the new mother, as someone who has gained a dependent through birth.
WOMEN ALREADY ENROLLED IN FULL-SCOPE OR EXPANSION MEDICAID
You May Like: How To Make A Newborn Baby Stop Crying
Does Private Insurance Also Cover A Newborn
It depends. Small group employer-sponsored plans must include the EHBs, including maternity and newborn care, but large group and self-insured employer-sponsored plans are exempt from this requirement. While the requirement for newborn care covers childbirth and immediate care following birth, women must enroll their babies in coverage soon after birth.
I Am A Health First Colorado Or Child Health Plan Plus Member And I Just Had A Baby How Do I Get Health Care Coverage For My Newborn
If you are a woman enrolled in Health First Colorado or Child Health Plan Plus when your baby is born, you can add your newborn to your case online by reporting a change through your PEAK account at Colorado.gov/PEAK, or using the Health First Colorado mobile app. Your baby will then be automatically enrolled in health coverage until his or her first birthday.
You also have the option to report the birth of your baby to your county of residence human services office or a Medical Assistance site case worker near you. Once your baby is added to your case and you have their State ID, you are able to take your baby to the doctor.
More Topics
Recommended Reading: When Can You Do A Dna Test On A Newborn
Important Facts When Adopting
Contact your health plan or your spouses health plan as soon as possible to find out how to enroll your child in group health plan coverage.
As long as you enroll your child within 30 days of adoption or placement for adoption, coverage should be effective as of your childs adoption or placement date and your child cannot be subject to a preexisting condition exclusion.
Remember, you should enroll your child within 30 days of the date of adoption or placement for adoption.
Do Marketplace Health Plans Provide Women With Comprehensive Coverage Including Maternity Care
Yes. All Marketplace plans must include the ten Essential Health Benefits , one of which is maternity and newborn care. HHS has not specified what must be covered under this category, delegating that authority to the states. Thus, specific benefits covered under maternity care vary by state.
2. What changes when a woman enrolled in a Marketplace plan becomes pregnant?
Nothing, unless she wants it to. The woman may choose to remain in a Marketplace plan or, if eligible, to enroll in Medicaid or CHIP. The woman will not lose eligibility for the APTCs as a result of access to MEC through full-scope or pregnancy-related Medicaid, but cannot be enrolled in both simultaneously and thus must choose. In deciding which coverage to select, overall cost, access to preferred providers, impact of transitioning across plans, and effect on family coverage influence preference.
Read Also: How To Soothe Newborn Constipation
Medicaid In New York State
- COVID-19 News and Updates:
- COVID Information for Medicaid Consumers:
- Medicaid Coverage through Your Local Department of Social Services during the Coronavirus Emergency –
- Medicaid Telehealth Services During the Coronavirus Emergency –
- IRS Form 1095-B Update:
- The 1095-B form for Tax Year 2020 is no longer being mailed automatically.If you need a copy of your 1095-B for Tax Year 2020, you can request it:
- By e-mail – or
Your Protections Under The Newborns And Mothers Health Protection Act
If a group health plan, health insurance company, or health maintenance organization provides maternity benefits, it may not restrict benefits for a hospital stay in connection with childbirth to less than 48 hours following a vaginal delivery or 96 hours following a delivery by cesarean section.
You cannot be required to obtain preauthorization from your plan in order for your 48-hour or 96-hour stay to be covered.
The law allows you and your baby to be released earlier than these time periods only if the attending provider decides, after consulting with you, that you or your baby can be discharged earlier.
In any case, the attending provider cannot receive incentives or disincentives to discharge you or your child earlier than 48 hours .
If your state has a law that provides similar hospital stay protections and your plan offers coverage through an insurance policy or HMO, then you may be protected under state law rather than under the Newborns and Mothers Health Protection Act.
Also Check: How Many Times Should Newborn Eat
What If I Dont Have A Newborn Child Declaration Form
If you dont have a Newborn Child Declaration form, or if your baby is older than 52 weeks, you can use a Medicare enrolment application form. You will need your childs birth certificate and some supporting documents. You can mail or email the form to Medicare. Read more on the Services Australia website.
My Attending Provider Discharged Me In Less Than 48 Hours Is This Permissible
Yes. Under the Newborns Act an attending provider, after consulting with a mother, can discharge a mother or newborn in less than 48 hours. Your attending provider, after consulting with you, can decide to discharge you or your newborn earlier. However, it is not permissible for your plan or insurance company to offer you incentives to induce you to accept less than the minimum protections available to you under the Newborns Act. Further, it is not permissible for your plan or insurance company to provide incentives to induce your attending provider to discharge you or your newborn earlier than the minimum 48 hours after delivery .
Also Check: How To Release Gas From Stomach In Newborn Baby
Monitoring Substitution Of Coverage In Chip
States are required to include in their state plan a description of procedures used to ensure that CHIP coverage does not substitute for coverage under group health plans. States use various procedures to prevent substitution of coverage, such as monitoring survey data or private insurance databases, or applying a waiting period for individuals who are no longer enrolled in private coverage. This requirement can be found at section 2102 of the Social Security Act. Additional information on states specific CHIP waiting period policies.
Is It Permissible For My Health Plan Insurance Company Or Hmo To Require Me To Get Permission For A 48
No. Plans, insurance companies and HMOs cannot deny your coverage for the 48-hour hospital stay based on a failure to show medical necessity. However, plans, insurance companies, and HMOs can deny coverage for any portion of the stay that is longer than 48 hours based on their determination of whether it is medically necessary.
In addition, a plan may require you to give notice of pregnancy before admission to the hospital in order to obtain more favorable cost sharing. However, a plan may not reduce your benefits because your pregnancy began before the first day of coverage and you failed to give notice of the pregnancy before becoming covered under the plan. This type of plan provision operates as a preexisting condition exclusion and these exclusions cannot be applied to pregnancy.
Recommended Reading: Why Do Newborns Have Seizures
Can Uninsured Women Enroll In Marketplace Coverage Upon Becoming Pregnant
Only if it is within the established open enrollment period or a woman qualifies for a special enrollment period , does not have a plan that meets MEC through Medicaid or an employer, and meets income and immigration criteria. Note that except in the states of New York and Vermont, pregnancy does not trigger an SEP.
Under the ACA, people who do not qualify for Medicaid coverage that meets MEC, and have incomes between 100% and 400% FPL, qualify for advance premium tax credits and cost-sharing reductions , which they can use to reduce the cost of health insurance purchased through a Marketplace. Those with pregnancy-related Medicaid in the three states that do not constitute MEC are eligible for Marketplace subsidies. Certain lawfully-present immigrants with incomes under 100% FPL subject to Medicaids five-year ban in their state are also eligible for APTCs. Undocumented immigrants are not eligible for APTCs, CSRs, or Marketplace insurance.
Contact The Case Worker
You will need to contact your SNAP benefits case worker as soon as the baby is born. You may do this at the hospital or you may wait until you are home. Contacting your case worker may be simple or it may be incredibly difficult depending on their case load. Assuming you can reach them, they will guide you through the rest of the process. If you are unable to reach them you will need to take a few more proactive steps.
Also Check: Which Similac Formula Is Best For Newborns
How Long Does Medicaid Or Chip Coverage For Pregnancy Last
Medicaid or CHIP coverage based on pregnancy lasts through the postpartum period, ending on the last day of the month in which the 60-day postpartum period ends, regardless of income changes during that time. Once the postpartum period ends, the state must evaluate the womans eligibility for any other Medicaid coverage categories.
7. Is abortion covered by Medicaid or CHIP?
The Hyde Amendment, an annual requirement added by Congress to a federal appropriations bill, prohibits using federal funds abortion coverage except when a pregnancy results from rape or incest, or when continuing the pregnancy endangers the womans life. However, states may use their own funds to cover abortions, and 17 states currently do.
How Do I Know If The Newborns Act Protections Apply To My Coverage
Even if your plan offers benefits for hospital stays in connection with childbirth, the Newborns Act only applies to certain coverage. Specifically, it depends on whether your coverage is insured by an insurance company or HMO or self-insured by an employment-based plan. , the document that outlines your benefits and your rights under the plan, or contact your plan administrator to find out if your coverage in connection with childbirth is insured or self-insured.)
Self-insured coverage is subject to the Newborns’ Act. However, if your coverage is “insured” by an insurance company or HMO and your state has a similar law regulating coverage for newborns and mothers that meets specific criteria, then your rights will be the rights provided under state law rather than under the Newborns’ Act. The state law may differ slightly from the Newborns’ Act requirements, so it is important for you to know which law applies to your coverage in order to know what your rights are. Based on a preliminary analysis of state laws, most insured coverage is subject to state law requirements in lieu of the Federal protections.
Don’t Miss: Is It Common For Newborns To Fail Hearing Test
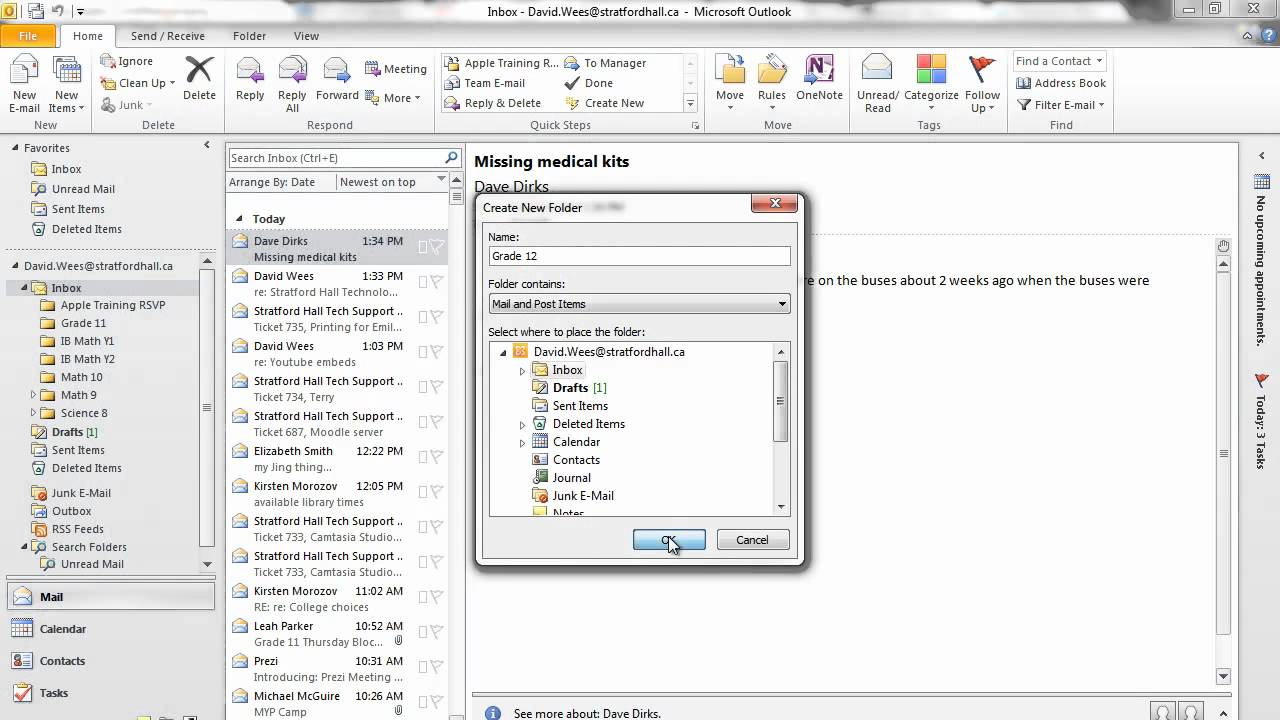
How To Add A Baby To Health Insurance
This article was co-authored by our trained team of editors and researchers who validated it for accuracy and comprehensiveness. wikiHow’s Content Management Team carefully monitors the work from our editorial staff to ensure that each article is backed by trusted research and meets our high quality standards. This article has been viewed 94,324 times.Learn more…
As you welcome a new baby into your family, you may be considering how you can ensure your new addition has health insurance coverage. If you have health insurance already through your employer or through a family health care plan, you can add your new baby to your existing health plan by following several steps.
Information On Title V
Title V prenatal care contractors may provide prenatal care and bill Title V for a maximum of the first two prenatal care visits for women who are in the process of applying for and enrolling in CHIP perinatal services. Title V contractors must inform, encourage, and assist pregnant women in the CHIP perinatal application process.
Please direct your questions or requests for additional information regarding Title V to
You May Like: How To Survive A Newborn
How Do I Apply For Medicaid
You can apply for Medicaid in any one of the following ways:
- Write, phone, or go to your .
- In New York City, contact the Human Resources Administration by calling 557-1399.
- Pregnant women and children can apply at many clinics, hospitals, and provider offices. Call your local department of social services to find out where you can apply.
> >
Do Medicaid And Chip Provide Pregnant Women With Comprehensive Health Coverage
Yes, in most but not all states. Full-scope Medicaid in every state provides comprehensive coverage, including prenatal care, labor and delivery, and any other medically necessary services.
Pregnancy-related Medicaid covers services necessary for the health of a pregnant woman and fetus, or that have become necessary as a result of the woman having been pregnant. Federal guidance from the Department of Health and Human Services clarified that the scope of covered services must be comprehensive because the womans health is intertwined with the fetus health, so it is difficult to determine which services are pregnancy-related. Federal statute requires coverage of prenatal care, delivery, postpartum care, and family planning, as well as services for conditions that may threaten carrying the fetus to full term or the fetus safe delivery. The state ultimately decides what broad set of services are covered. Forty-seven states provide pregnancy-related Medicaid that meets minimum essential coverage and thus is considered comprehensive. Pregnancy-related Medicaid in Arkansas, Idaho, and South Dakota does not meet MEC and is not comprehensive.
CHIP coverage for pregnant woman is also typically comprehensive. However, in states where services are being provided to the pregnant woman by covering the fetus, the services may not be comprehensive with respect to the health needs of the pregnant woman.
Recommended Reading: How Can I Get My Newborn To Sleep At Night
