Lead Screening Helps Keep Your Baby Safe From Lead Poisoning
Very young children are curious! They love to explore. But lead poisoning from lead paint, chips and dust, and lead in water, can interfere with growth, harm hearing, lower IQ scores and cause behavioral problems. There are usually no signs or symptoms until a child is seriously ill with lead poisoning. To check for lead poisoning, have a simple blood test for lead at regular appointments around your child’s first and second birthdays.
You can get an early start protecting your baby from lead by:
- Using cold tap water, not hot, to make infant formula. Let the cold water run for at least a minute to remove any lead picked up from the pipes.
- Using iron-fortified infant formula and cereals for toddlers, to help lower your baby’s lead risk.
- Washing your baby’s hands, pacifier and toys often.
- Being sure your toddler doesn’t put paint chips or plaster in his or her mouth, or chew on windowsills or stair rails.
- Damp mopping floors to remove lead dust.
- Keeping your toddler out of the house during any home renovations.
Setting Up Remittance Advice Receipt And Payment Options
The processing of most Medicaid transactions is performed by the eMedNY fiscal agent for the NYS Medicaid Program. eMedNY processes transactions 24 hours a day, 7 days a week and issues checks and remittance statements weekly, for processed claims.
Remittance Advices are generated every week for claims submitted from Thursday to Wednesday prior, and are available in multiple formats.
- Electronic Electronic remittances are issued in a HIPAA-compliant format known as the 835 or 820 therefore software is required to interpret the remittance information.
- PDF Remittance AdvicePDF version of the paper remittance is viewed with Adobe Reader® which is available free of charge. This Remittance Advice format may be downloaded and stored electronically. Additionally, it is not held with any corresponding paper Medicaid check for two weeks but released to you two weeks earlier. In order to receive the New York Medicaid paper remittance advice in a PDF format through eMedNY eXchange,
- Paper Medicaid checks and paper remittances are held for two weeks and two days before being issued to the provider.
ENQUIRIES: Questions should be directed to the eMedNY Call Center at 1-800-343-9000. Before submitting claims, providers may also phone the Call Center to request training from a eMedNY Regional Representative.
Determine How You Will Submit Claims To Emedny
Providers are given several options for submitting claims to eMedNY
Option 1: HIPAA Compliant Claim Formats Submitted Directly to eMedNY
Option 2: Medicaid’s Electronic Provider Assisted Claim Entry System web-based application
- Claims: Professional Institutional and Dental
- Claim Status Requests**
- Prior Approval Requests
- Eligibility Verification
*Real-time means that the claims are processed instantaneously and the provider can view the status of a real-time claim within seconds. There is no need to wait for a remittance statement to be mailed to find out about the status of submitted claims. **The status of claims submitted via the ePACES batch feature is generally available within 24 hours. To enroll in ePACES:
Option 3 Paper Claim Forms
Don’t Miss: How Much Sleep Is Too Much For A Newborn
Newborn Screening For Health Problems That Need Early Treatment
Some babies are born with health problems that can harm growth and development. Early treatment can keep babies healthy and further their development.
In New York State, all babies are tested at birth for seven health problems. To do this, a tiny blood sample will be taken from the baby’s heel before he or she goes home.
You will get your baby’s test results only if there is a problem. You may be asked to have your baby retested. Don’t panic. It’s more likely a problem with the blood test, not the baby.
You Have Two Ways To Apply For Chip
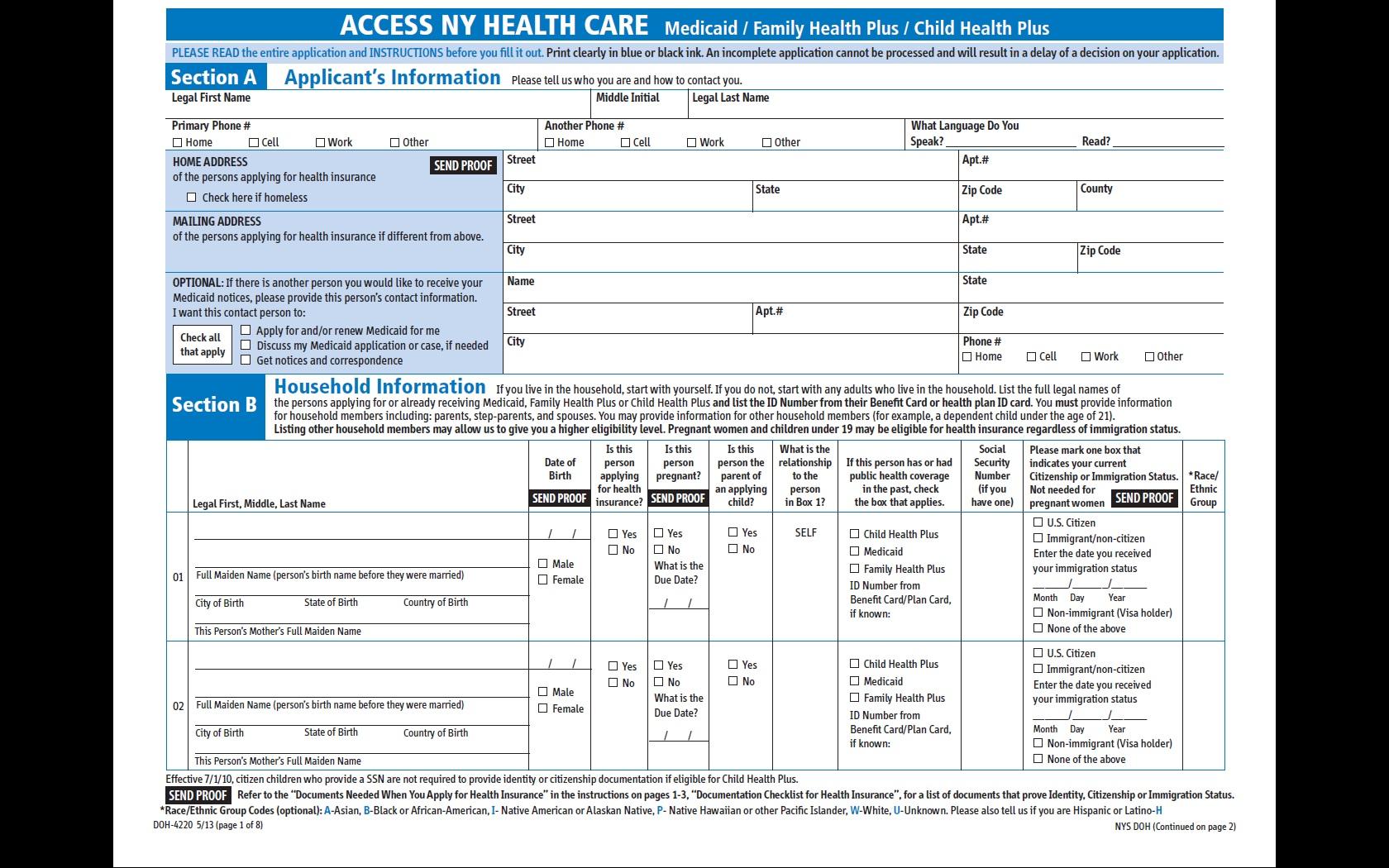
. HHS has not specified what must be. In accordance with New York Insurance Law 4305 McKinney 2007 if the insured parent does not add the newborn infant to the coverage within 30 days the newborn infant would be covered only for the period specified in Insurance Law 4303. Medisource Fidelis Amerigroup Yourcare Wellcare and Medicaid.
I understand that the state may ask me for more information. New Yorks Medicaid program provides comprehensive health coverage to more than 73 million lower-income New Yorkers as of December 2021 Medicaid pays for a wide-range of services depending on your age financial circumstances family situation or living arrangements. If Medicaid was obtained through NYS of Health you must contact them at 855 355-5777 or via their website at.
Find a program by state or call the Health Insurance Marketplace at 1-800-318-2596 TTY. To be eligible you should be able to answer yes to these questions. CHIP is administered by states according to federal requirements.
To get a copy of the form mailed to you call the New York State Medicaid Help Line at 1-800-541-2831. Out here you have to sign up for medicaid before your baby is born and then they give you a piece of paper to fill out at the hospital after the baby is born. The account holder must mark Yes to the financial assistance question.
How To Add Newborn To Medicaid NyClick on your provider manual below and read. Add your newborn to your insurance plan. There is no pre-enrollment.
Health Ny Gov
Don’t Miss: Is It Normal For Newborns To Cry A Lot
Using Your Healthy Connections Plan
Q. What medical services does Medicaid cover? A. Within certain limits, Medicaid will pay for services that are medically necessary. Examples of services that may be covered include doctor visits, medications, hospital visits, and many other medical services.
If you have any questions about what is covered, to view a chart that shows each health plan and what they cover. You can also contact Healthy Connections toll-free at 1-888-549-0820.
Q. How long will my Medicaid benefits remain active? A. Eligibility for most Healthy Connections programs lasts for 1 year. After 1 year, South Carolina Health and Human Services will review your case annually.
Q. I was enrolled in S.C. Healthy Connections Choices and now am told I must choose between health plans. What should I do? A. The Healthy Connections Choices website offers comprehensive information on its health plans. Members may utilize a Quick Start Guide, search for doctors, compare plans, and more. Please visit S.C. Healthy Connections Choices for more information.
Q. Do I need to tell South Carolina Healthy Connections when I move or change jobs? A. Yes. If you have any changes to your income, resources, living arrangements, address or anything else that might affect your eligibility you must report these changes to Healthy Connections right away at 1-888-549-0820.
Q. What if my Medicaid card is lost or stolen? A. Report a lost or stolen card to Healthy Connections immediately at 1-888-549-0820.
Relevant Rule: Wac 182
- Newborn children may be enrolled in medical and dental coverage upon birth and adopted children may be enrolled when the employee assumes legal obligation for total or partial support in anticipation of adoption. If enrolling the newborn in medical and or dental coverage, the child’s coverage will begin on the date of birth. If enrolling a newly adopted child, coverage will begin on the date of placement or the date a legal obligation is assumed in anticipation of adoption, whichever is earlier.
- If the employee previously waived medical coverage, he/she must enroll in medical to add an eligible dependent to medical coverage. Coverage for the employee begins the first day of the month in which the event occurs.
- To enroll a spouse or state registered domestic partner of an employee, coverage will begin the first day of the month in which the event occurs.
You May Like: Are Newborn And Size 1 Diapers The Same
The Sc Department Of Health And Environmental Control Newborn Screening Program Currently Screens For 53 Disorders
How to add newborn to medicaid sc. Will a marketplace health plan also cover a newborn. Family connection of sc makes every effort to ensure that our website is 508 compliant, as well as useable by anyone who visits us. If youre eligible, youll receive a medical id card with your approval notice.
The omnibus budget reconciliation act of 1986 gave states the option to provide medicaid coverage to pregnant women with low income. Why don’t you look at the history of a beneficiary and assign them based on providers they already see? Chip covers birth through age 18 unless otherwise noted in parentheses.
Once the newborn’s name is updated on file, a new medicaid gold card is. Chip is administered by states, according to federal requirements. In a health plan, you get the same benefits as regular medicaid.
Within two working days after after a completed submission through the portal, the medicaid fiscal agent will update the newborn’s name, gender, and birth date and activate the coverage. If you are a woman enrolled in health first colorado or child health plan plus when your baby is born, you can add your newborn to your case online by reporting a change through your peak account at colorado.gov/peak, or using the health first colorado mobile app. The state plan stipulates equitable distribution of membership into the plans, the assignment process is automated.
Community Resource Guide
Unitedhealthcare Senior Care Options Plan
UnitedHealthcare SCO is a Coordinated Care plan with a Medicare contract and a contract with the Commonwealth of Massachusetts Medicaid program. Enrollment in the plan depends on the plans contract renewal with Medicare. This plan is a voluntary program that is available to anyone 65 and older who qualifies for MassHealth Standard and Original Medicare. If you have MassHealth Standard, but you do not qualify for Original Medicare, you may still be eligible to enroll in our MassHealth Senior Care Option plan and receive all of your MassHealth benefits through our SCO program.
You May Like: How To Help A Gassy Newborn Sleep
Notification Of Determination By Nys Doh
A written determination of approval or denial of the submitted application will be sent to the provider.
If the application is approved, a letter containing the provider’s MMIS ID Number, the effective date when services may be provided to an enrolled client, and other information related to their enrollment will be sent to the enrollee.
Maintaining Your Medicaid Coverage
If you fail to report life changes you could lose your Medicaid coverage, even if those changes don’t actually impact your eligibility.
Recommended Reading: How To Avoid Colic In Newborn
Unitedhealthcare Dual Complete Plans
Plans are insured through UnitedHealthcare Insurance Company or one of its affiliated companies, a Medicare Advantage organization with a Medicare contract and a contract with the State Medicaid Program. Enrollment in the plan depends on the plans contract renewal with Medicare. This plan is available to anyone who has both Medical Assistance from the State and Medicare. This information is not a complete description of benefits. Call TTY 711 for more information. Limitations, co-payments, and restrictions may apply. Benefits, premiums and/or co-payments/co-insurance may change on January 1 of each year.
If You May Qualify For Medicaid Or Childrens Health Insurance Program
- Medicaid and CHIP provide free or low-cost health coverage to millions of Americans, including some low-income people, families and children, and pregnant women.
- Eligibility for these programs depends on your household size, income, and citizenship or immigration status. Specific rules and benefits vary by state.
- You can apply for Medicaid or CHIP any time during the year, not just during the annual Open Enrollment Period.
- You can apply 2 ways: Directly through your state agency, or by filling out a Marketplace application and selecting that you want help paying for coverage.
- Learn how to apply for Medicaid and CHIP.
You May Like: How Much Ml Should A Newborn Eat
If You Dont Have Health Coverage
- Health coverage makes it easier to get the medical check-ups and screening tests to help keep both you and your baby healthy during pregnancy.
- If you qualify for a Special Enrollment Period due to a life event like moving or losing other coverage, you may be able to enroll in a Marketplace health plan right now. Being pregnant doesnt make you eligible, but the birth of a child does.
- Create an account now to apply for Marketplace coverage through the Open Enrollment Period or a Special Enrollment Period. If you select the option to get help paying for coverage on your application, youll be asked if youre pregnant. Reporting your pregnancy may help you and your family members get the most affordable coverage.
- If you dont qualify for a Special Enrollment Period right now, youll be eligible to apply within 60 days of your childs birth. You can also enroll in 2021 coverage during the next Open Enrollment Period this fall.
- If eligible for Medicaid or CHIP, your coverage can begin at any time.
