Newborn Screening For Chip And Chip Perinatal
Providers submitting newborn screening specimens to the Department of State Health Services laboratory use the NBS3: Medicaid/Charity Care/CHIP test card when screening babies insured by CHIP and CHIP Perinatal. This test card is available at no charge.
Process
- The provider sends a request for the NBS3: Medicaid/charity care/CHIP test cards from the DSHS laboratory.
- The DSHS laboratory sends the provider the test cards.
- The provider draws the infant’s blood sample, and completes the test card.
- The provider sends the test kit to the DSHS laboratory for analysis.
- The DSHS laboratory conducts the screen for genetic disorders.
- The DSHS laboratory notifies the provider of the results.
Income Requirements For Florida Medicaid
There are income requirements for Medicaid in Florida. You need to earn an income that is within the federal poverty level for your group. This is calculated by a specific system that is known as the Modified Adjusted Gross Income, or MAGI.
Basically, before taxes, income needs to be under these amounts, according to Benefits.gov:
Household Size Maximum Income Level
1 $15,000
- Speech-language pathology, respiratory, physical, and occupational therapy services
Information On Title V
Title V prenatal care contractors may provide prenatal care and bill Title V for a maximum of the first two prenatal care visits for women who are in the process of applying for and enrolling in CHIP perinatal services. Title V contractors must inform, encourage, and assist pregnant women in the CHIP perinatal application process.
Please direct your questions or requests for additional information regarding Title V to
Also Check: Why Do Newborns Spit Up Breast Milk
Ways To Apply For Chip:
- Fill out an application through the Health Insurance Marketplace®. If it looks like anyone in your household qualifies for Medicaid or CHIP, well send your information to your state agency. Theyll contact you about enrollment. When you submit your Marketplace application, youll also find out if you qualify for an individual insurance plan with savings based on your income instead. Create an account or log in to an existing account to get started.
FYI: Apply any time
You can apply for and enroll in Medicaid or CHIP any time of year. Theres no limited enrollment period for either Medicaid or CHIP. If you qualify, your coverage can start immediately.
Lawfully Residing Targeted Low
States have the option to provide CHIP and Medicaid coverage to children and pregnant women who are lawfully residing in the United States and are otherwise eligible for coverage, including those within their first five years of having certain legal status. If states do not adopt this option, federal law requires a 5-year waiting period before many legal immigrants are permitted to enroll in Medicaid and CHIP. Learn more about providing health coverage to lawfully residing children and pregnant women at 2107 of the Social Security Act, and in SHO# 10-006 . A list of states providing Medicaid and CHIP coverage to lawfully residing children and/or pregnant women.
You May Like: When Can You Take A Newborn Out For A Walk
How Does A Woman Enroll In A Chip Perinatal Health Plan
Once a woman is found to be eligible for CHIP perinatal services, her unborn child must be enrolled in a health plan. The woman has 15 calendar days to select a health plan. The 15-day window opens the day she receives a letter from HHSC saying she qualifies for CHIP perinatal services on behalf of her unborn child. If she does not choose a health plan within the 15-day timeframe, HHS will choose one for her.
Once she has enrolled, the woman will receive an ID card from her health plan that specifies CHIP Perinatal Program.
What Services Are Not Covered
CHIP perinatal provides a basic prenatal care package. Participating health plans will distribute a provider manual that includes covered and non-covered benefits. Below are examples of non-covered services:
- Inpatient hospital care for the mother of the unborn child that is not related to labor with delivery, such as a serious injury, illness and more
- Labor without delivery of the baby
- Most outpatient specialty services, such as mental health and substance abuse treatment, asthma management, and cardiac care
A pregnant woman may apply for Emergency Medicaid in emergency situations. However, the bar-coded Form H3038-P that HHS mails to a pregnant woman with income at or below 198 percent of the FPL only may be used to apply for Emergency Medicaid for her labor with delivery. She may not use her bar-coded H3038-P, mailed by HHS, for services such as:
- Labor with no delivery
- Other non-delivery emergency services, such as hospitalization for a serious injury, illness and more
You May Like: When Can You Wash A Newborn
What Other Documents Do Women Need To Send With Their Application
Women applying for CHIP perinatal services need to submit the following documents of proof:
Proof of Income
Proof must show current income for each person in the home. Proof can be:
- Pay check stub from the last 60 days showing pay before taxes or deductions
- Last year’s tax return
- Proof of self-employment
- Letter from your employer. This letter takes the place of a paycheck stub. It should how much you make now and how often you get paid. It also should include your name, the employer’s name, and the employer’s signature.
- Social Security statement
Austin, TX 78714-9968
In person
Finished applications and copies of required information can be turned in to a local HHS benefits office. To find the office nearest you, call 2-1-1 or 877-541-7905 after you pick a language, press 2.
What Are The Benefits Once The Child Is Born
- Two postpartum visits for the mother.
- Once a child is discharged from the initial hospital admission, the child receives the traditional CHIP benefit package, or Medicaid, depending on their income. CHIP or Medicaid benefits include regular checkups, immunizations and prescriptions for the baby after he or she leaves the hospital.
- Depending on income, the newborn may get Medicaid from birth to their 1st birthday. Most CHIP perinatal infants qualify for Medicaid. If the baby is eligible to get Medicaid, the mother will receive a letter and Form H3038-P, CHIP Perinatal – Emergency Medical Services Certification, in the mail before delivery.
You May Like: How Do You Get Medicaid For A Newborn
How Do I Know Who To Bill
Claims for the Mother
Facilities
- Facilities that need to bill TMHP should look at the patient’s CHIP perinatal health plan ID card. It should have TMHP or Medicaid Claims Administrator under Hospital Facility Billing.
- Facilities that need to bill the CHIP perinatal health plan should find the health plan’s name under Hospital Facility Billing.
Professional charges
How Long Does The Eligibility And Enrollment Process Take
Texas Health and Human Services staff have 15 business days to process the application from the day they received it. Once eligibility is determined, the pregnant woman enrolls in a CHIP perinatal health plan on behalf of her unborn child. She has 15 calendar days to select a health plan from the day she gets a letter stating she can get CHIP perinatal benefits. If she does not choose a medical plan within the 15-day timeframe, HHS will choose one for her.
Also Check: Which Similac Formula Is Best For Newborns
How Does The Medically Needy Spend
Medically Needy provides Medicaid eligibility to qualified individuals and families who may have too much income to qualify for regular Medicaid programs. Individuals and families who meet all Medicaid program requirements, except that their income is above those program limits, can spend-down or reduce their income to Medicaid eligibility levels using incurred medical expenses.
How Do I Apply For Medicaid
You can apply for Medicaid in any one of the following ways:
- Write, phone, or go to your .
- In New York City, contact the Human Resources Administration by calling 557-1399.
- Pregnant women and children can apply at many clinics, hospitals, and provider offices. Call your local department of social services to find out where you can apply.
> >
Recommended Reading: How Much To Feed Newborn Baby Formula
Serving Mississippians In Need
The Mississippi Division of Medicaid serves a variety of Mississippi populations through three main coverage groups: Regular fee-for-service Medicaid, Medicaids coordinated care program MississippiCAN, and the Childrens Health Insurance Program .
DOM serves roughly one in four Mississippians who receive health benefits through Medicaid or CHIP.
For individuals who have qualified for Mississippi Medicaid benefits, the following links will provide more information regarding service copays, how to find a provider, reporting changes and more.
- Copay Information some medical services may require a copay or small fee
- Provider search search to locate a provider who accepts Mississippi Medicaid
- Envision website portal for Mississippi Medicaid beneficiary services
Pregnant Women And Infants
Healthy Connections provides coverage to pregnant women with low income. This coverage for the mother continues for 60 days after the baby’s birth. The infant is covered up to age one.
A woman who may qualify for this program must:
- Be pregnant
- Be a South Carolina resident
- Be a U.S. citizen or Lawful Permanent Resident Alien
- Have a Social Security number or verify an application for one
Individuals who are eligible will receive all Medicaid covered services.
Apply online or complete the following form and submit it electronically to , by mail to SCDHHS-Central Mail, P.O. Box 100101, Columbia, SC 29202-3101 or to your .
The Omnibus Budget Reconciliation Act of 1986 gave states the option to provide Medicaid coverage to pregnant women with low income.
Read Also: How Often To Check Newborn Diaper
How Are Providers Reimbursed What Are The Reimbursement Rates
To be reimbursed, providers must participate in a health plan’s network. Reimbursement rates will be negotiated between the provider and the health plan per contractual agreements. Providers will submit claims directly to the health plan for payment. Claim forms and processes vary by health plan. Consult the CHIP perinatal health plan for billing details.
What If I See A Chip Perinatal Newborn Who Has Not Yet Been Issued A Unique Id Card
Because most CHIP perinatal newborns change to Medicaid from their date of birth, their moms typically need to enroll the baby in a STAR health plan after they are born. Once enrolled, they will receive a new STAR health plan ID, as well as a Your Texas Benefits Medicaid card. Even if the baby does not have a Medicaid card or a STAR health plan ID, you can verify the baby’s Medicaid eligibility by doing one of the following:
- Go to TexMedConnect on the TMHP website
There is a gap between the time the child is born and he or she is enrolled in a STAR health plan. During this gap, newborn claims will be paid with traditional, fee-for-service Medicaid.
For babies who remain in CHIP perinatal after birth, contact the health plan that provided prenatal care under CHIP perinatal.
You May Like: Why Do Newborns Cry For No Reason
If You Qualify Under A Non
- If you are a U.S. citizen and provide a valid Social Security Number , a match with the Social Security Administration will verify your SSN, date of birth and U.S. citizenship. If SSA verifies this information, no further proof is needed. The SSA match cannot verify birth information for a naturalized citizen. You will need to submit proof of naturalization or a U.S. passport.
- Proof of citizenship or immigration status*
- Proof of age , like a birth certificate
- Four weeks of recent paycheck stubs
- Proof of your income from sources like Social Security, Veteran´s Benefits , retirement benefits, Unemployment Insurance Benefits , Child Support payments
- If you are age 65 or older, or certified blind or disabled, and applying for nursing home care waivered services, or other community based long term care services, you need to provide information on bank accounts, insurance policies and other resources
- Proof of where you live, such as a rent receipt, landlord statement, mortgage statement, or envelope from mail you received recently
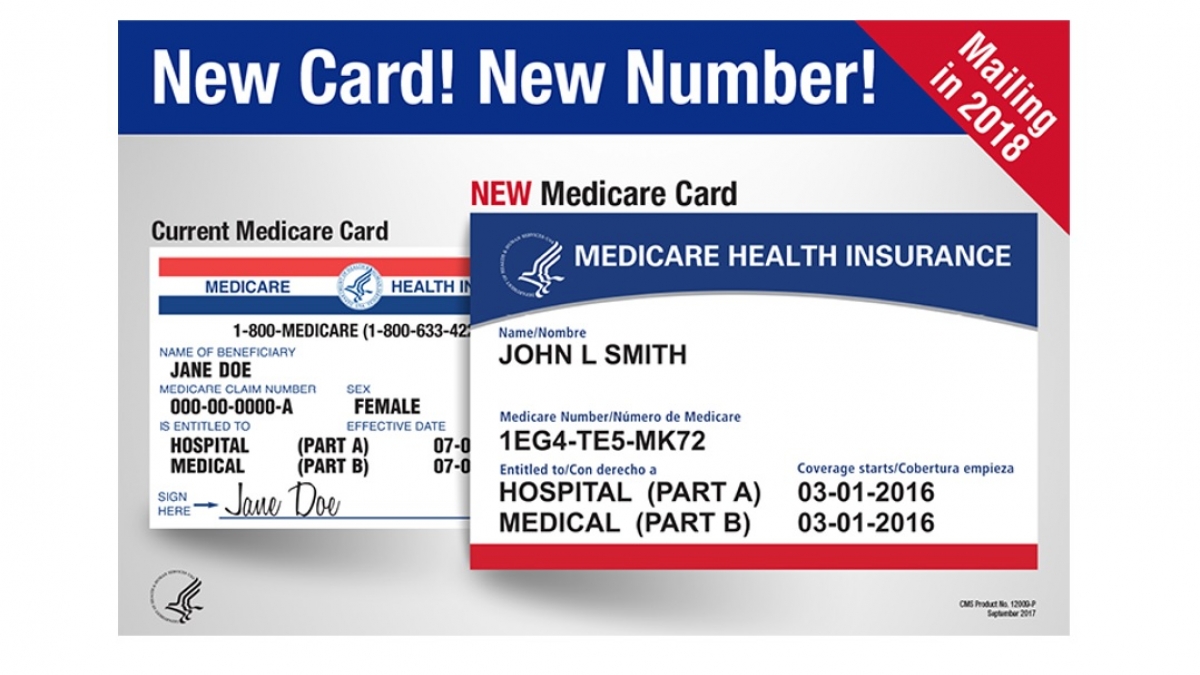
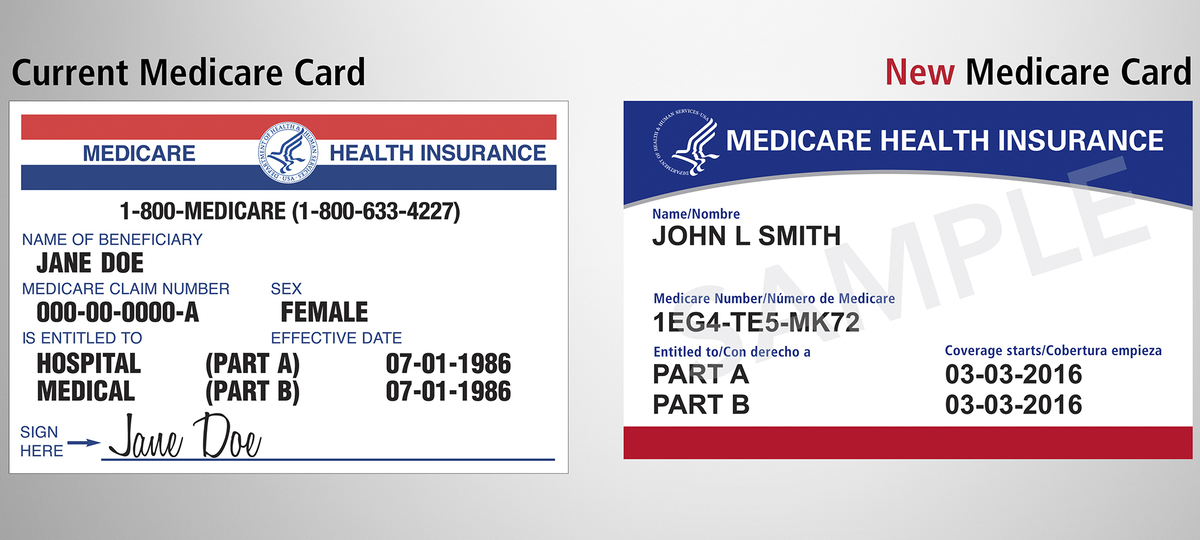
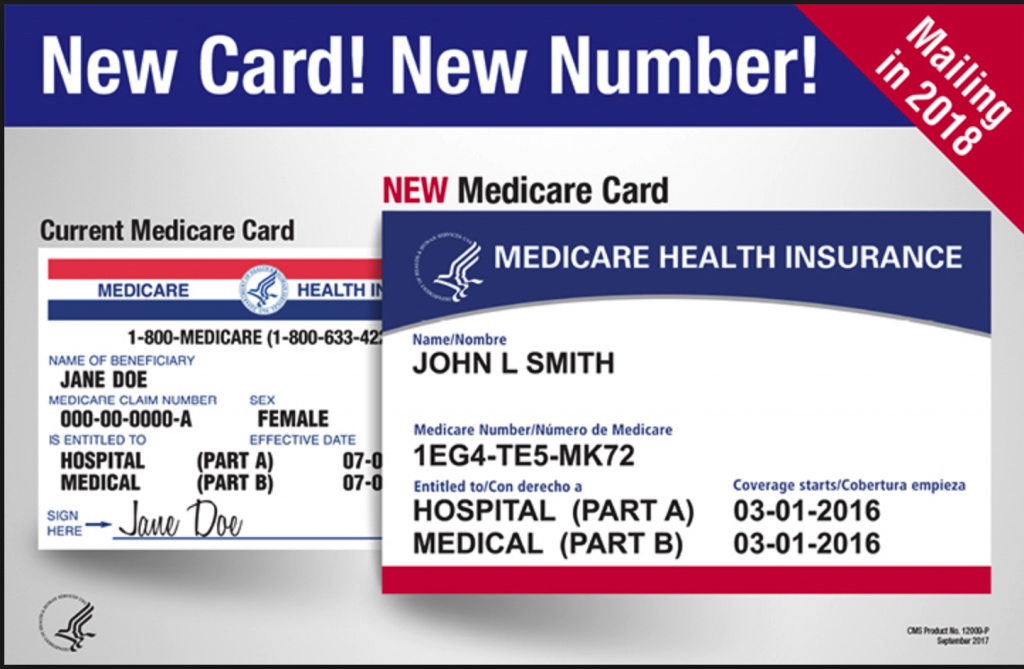
- Insurance benefit card or the policy
- Medicare Benefit Card **
Proof of Medicare application can be:
- Your award or denial letter from the Social Security Administration, OR
- Your on-line confirmation letter stating that you have applied for Medicare with the Social Security Administration.
Apply Now:
The following are exempt from all Medicaid co-payments:
What If I Think A Decision You Make Is Unfair Incorrect Or Made Too Late
You have the right to appeal the Medicaid decision. There are several ways to request an appeal. You can write the reason you disagree with the decision on the back of the decision letter and then mail or fax it to Medicaid as directed on the letter. You can also fax the decision letter to the Division of Administrative Law at 225-219-9823 or mail it to the Division of Administrative Law, Department of Health Section, P. O. Box 4189, Baton Rouge, LA 70821-4183. You can request an appeal by phone by calling Medicaid Customer Service at 1-888-342-6207 or the Division of Administrative Law at 225-342-5800.
Don’t Miss: How To Soothe A Newborn To Sleep
Provider Inquiry Newborn Spreadsheet
If you know the mother is pregnant, Medicaid eligible, and her unborn child does not have a number, you may have the baby added by emailing a password protected Master Unborn Provider Spreadsheet to the statewide DCF email address identified on the spreadsheet. This spreadsheet can also be used to contact DCF to request assistance regarding missing eligibility for newborns or issues concerning incorrect demographics such as discrepancies in dates of birth.
Please review the Provider Unborn Update Spreadsheet Completion Guide for further instructions on completing and submitting inquiries to DCF.
Services Covered By Medicaid And Chip
- Regular checkups at the doctor and dentist
- Medicine and vaccines
- Access to medical specialists and mental health care
- Treatment of special health needs and pre-existing conditions
These services are provided by health plans. If your child gets Medicaid or CHIP, you will choose a plan from the ones available in your service area.
You May Like: How Often Do Newborns Need A Bath
Healthcare Coverage For Your Baby
If your child is lives in a family with an income at or below the Medicaid eligibility level, your newborn will be enrolled in Medicaid for 12 months of continuous Medicaid coverage beginning on his or her date of birth. After the twelve months of coverage ends, you can apply through the state CHIP office to have your baby covered under the CHIP program. Learn how to apply for Medicaid services.
Monitoring Substitution Of Coverage In Chip
States are required to include in their state plan a description of procedures used to ensure that CHIP coverage does not substitute for coverage under group health plans. States use various procedures to prevent substitution of coverage, such as monitoring survey data or private insurance databases, or applying a waiting period for individuals who are no longer enrolled in private coverage. This requirement can be found at section 2102 of the Social Security Act. Additional information on states specific CHIP waiting period policies.
Read Also: How Much Will A Newborn Sleep
